Jail Populations Mental Health Substance Abuse May 23, 2023
Since 2015, Policy Research, Inc. (PRI) has partnered with MacArthur’s Safety and Justice Challenge (SJC) to reduce the number of individuals involved, or at risk of involvement with, the criminal legal system who have mental illness, substance use, and other complex needs. Studies highlight the importance of concentrating on this population as communities work to tackle the misuse and overuse of jails and create more equitable systems:
- About 5% of the general population has a Serious Mental Illness (SMI), compared with 5% of men and 31% of women incarcerated in local jails. An even greater percentage of both groups lives with broader mental health needs and are prescribed psychotropic medication.
- 63% of those incarcerated in jail have a substance use disorder.
- People with mental illness often remain in jail longer than individuals without.
- Despite overall jail population reductions in the last few years, many communities participating in the Safety and Justice Challenge have seen the proportion of individuals with mental illness increase.
- Despite stigmatizing myths, the majority of individuals with mental illness are not violent and the majority of violent acts are not committed by those with mental illness.
As part of the Safety and Justice Challenge, PRI created the IMPACT Network to provide technical assistance to participating communities on issues related to the over-incarceration of individuals with mental illness and substance use disorders. The IMPACT Network communities engage in a peer-to-peer learning model to accelerate best and promising practices in behavioral health reform and jail diversion, with a commitment to pursuing community-driven, race-conscious solutions to reduce harm to populations overrepresented in, or disparately impacted by, the criminal legal system.
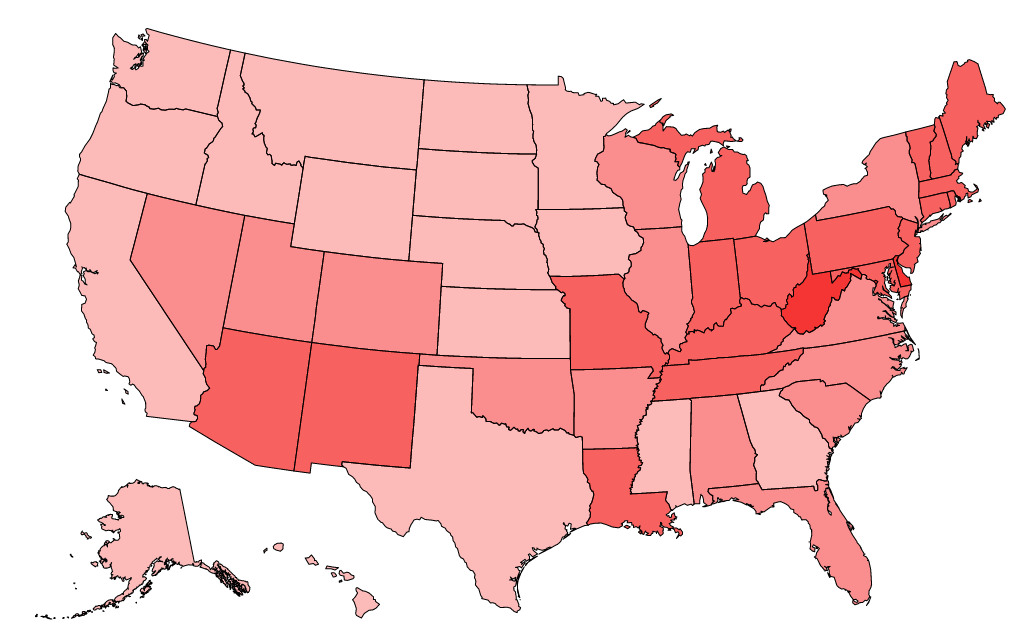
The SJC IMPACT Network began in 2021 with a group of 11 jurisdictions.
Over the past two years, these communities have participated in topical technical assistance meetings focused on behavioral health data tracking and evaluation, equity within the intersection of the criminal legal system and behavioral health, developing early diversion strategies, building a robust jail continuum of care, and other critical topics.
The communities participating in the IMPACT Network focus on a variety of strategies to decrease inappropriate incarceration of people with behavioral health needs.
Allegheny County, PA
Allegheny County’s Justice Related Services (JRS) provides assessment, treatment placement, and service coordination to court-involved individuals with mental health or co-occurring diagnoses. They are also focusing on balancing risk and needs during decision making for people with behavioral health needs, developing alternative response to certain 911 calls, and building out a broader continuum of peer supports for court-involved people.
Orange County, CA
In April 2022, the Orange County District Attorney’s Office launched their Focused Intervention Route to Services and Treatment (FIRST Point) pre-filing diversion pilot program. The pilot program connects people who have committed low-level crimes with services to address mental health and substance use issues to ensure a criminal proceeding does not inhibit future work and education opportunities.
San Juan County, NM
San Juan County has worked closely with community stakeholders and cross-agency representatives through their Sequential Intercept Mapping (SIM) process, identifying gaps in services available to individuals with behavioral health needs. As part of their post-SIM work, the county plans to identify a system for data collection that will assist stakeholders in tracking the county needs and build planning capacity toward creation of a mental health drop-in center.
In early 2023, PRI expanded the IMPACT Network by adding six additional communities: Doña Ana County, NM; Solano County, CA; Sarpy County, NE; Douglas County, NE; Issaquah, WA; and Natrona County, WY, for a total of 17 jurisdictions. This new group of counties brings to the IMPACT Network communities from the West and Midwest, including several smaller and more rural jurisdictions.
We are excited to further diversify the IMPACT Network and continue this important work toward the goals of reimagining systems, reducing the footprint of local jails, and increasing equity.